Is knowing really worth it?
BY CAROL BRADLEY BURSACK | 2.3.2017
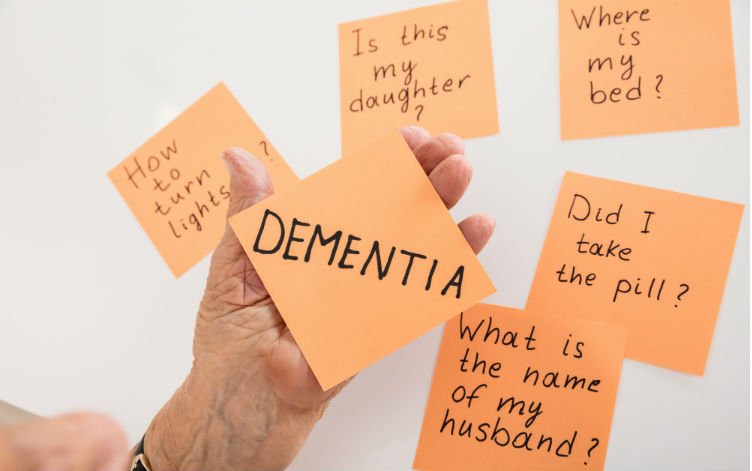
Many people understandably wonder if there is any point in seeking an official diagnosis for Alzheimer’s disease or other types of dementia when there is no cure and doctors are limited in how much they can help manage the symptoms. While this kind of thinking is practical in some ways, it can have terrible consequences for a person experiencing cognitive issues (and their family members). Even a general diagnosis can aid families in getting practical help for their loved ones and open up educational opportunities to help them through the difficult territory of dementia care. It can also ensure they are receiving appropriate medical care and help to prevent elder abuse.
I approached Dr. Elizabeth Landsverk, Adjunct Clinical Professor at the Stanford University School of Medicine and Medical Director at Silverado Senior Living in Belmont, CA, about the dangers of allowing cognitive changes go undiagnosed. Below, Dr. Landsverk shares a personal story along with some wise words of advice for all of us.
A Cautionary Tale
“My friend, Rhonda, went through quite an ordeal recently due to undetected mental decline in her mother, Sue. Sue lived in upstate Minnesota in a house that she had been in for 40 years, and Rhonda lived about 2,000 miles away in California. The only local family Sue had was a granddaughter, Jane.
“Sue had been doing well until a few years ago when she began forgetting to take her medications and go to appointments. Jane eventually moved in with Sue to help, and this arrangement seemed to go smoothly for a while. Rhonda had asked her mother to move to California to be with her, but each time Sue would refuse, saying she was fine and that Jane was helping her. This went on until last year when everything changed.
“Jane took her grandmother to Florida to sign a mortgage on a house for her. Sue’s cat was taken along on the trip and somehow got lost in Tennessee. Jane took Sue home to Minnesota and told her she’d drive back to Tennessee to ‘find her cat.’
“During this time, another friend of mine, Meg, who knew both Sue and Jane, visited Sue and was distraught by what she found. Meg called Rhonda and told her that her mother was dehydrated and confused and that Jane needed to fly back to Minnesota immediately. Meg brought Sue to her own home and we both ensured she was taken care of.
“It soon became obvious that Jane was never coming back. She had previously told Rhonda that Sue had no medical issues and took no medications, but a bag of prescriptions in Sue’s home told a very different story. Sue had been treated for emphysema, high blood pressure, and cholesterol, and she also took Ambien and some Tylenol PM for sleep. Sue seemed frail and anxious and could not tell me what had happened in the past month with Jane. She didn’t ask where Rhonda was or about the new home or even her missing cat.
“Several weeks later, Sue became increasingly short of breath due to a respiratory infection and ended up in the hospital. A chest x-ray showed that she had a tumor in her chest. We finally got Sue’s primary doctor onboard and I was able to see her medical records. It turns out that she had been diagnosed with lung cancer more than a year earlier! Sue declined quickly and died from within six months. By that time, most of her money was gone, as was ownership of her house.
“The other side of this story is that Jane was addicted to drugs and had asked her grandmother to sign over the title of the house to her. Jane was supposed to be taking care of Sue’s medical issues, but did not even bother to get Sue any cancer treatments. (Although Jane did buy a life insurance policy on her.)”
A Diagnosis Can Have Medical Consequences
“Sadly, my story is not an isolated issue. Rather, it is the challenge of our age. In the 1960s, the average life span was 61 years. Now that average has risen to 78 for men and 83 for women. We are living much longer. The incidence of dementia is 10 percent at age 65 but grows to 30-50 percent by age 85. Longer lifespans are the cause of the rapid growth of dementia in our communities. Many of the people who live with this condition remain undiagnosed, which leaves them incredibly vulnerable.
“It is best to have neuropsychological testing done as soon as there are any signs of cognitive decline. In Sue’s case, her increasing forgetfulness was a major red flag, even though she likely downplayed it. If your loved one doesn’t have a psychologist, ask their primary care physician for a referral. If there isn’t one available in your area, contact the nearest medical center or geriatric center.
“Another important reason why families should seek a diagnosis as early as possible is because symptoms of dementia, such as confusion, impaired judgement, behavioral issues, and communication problems, can be caused by other less serious and REVERSIBLE health issues. Simply blaming “old age” for these symptoms can delay proper treatment and increase the risk of permanent damage to the body and the mind. Normal pressure hydrocephalus (NPH), depression, medication side effects and interactions, urinary tract infections (UTIs), thyroid problems, diabetes, and certain vitamin deficiencies can all cause symptoms that are similar to Alzheimer’s disease and other types of dementia. Depending on the diagnosis, a course of antibiotics, a close look at a loved one medications, or a healthier diet could make all the difference.
“Even if the conclusion is still some form of dementia, if it is caught early enough, the family can work together to ensure all their affairs are in order, make plans for the future while there is still time, and protect their loved one from situations and people they are no longer capable of handling. If an individual’s condition deteriorates far enough before being addressed, then their family members may have to go through the long and expensive process of obtaining guardianship. Lastly, although the treatment options for dementia are limited, medications can also help to minimize some symptoms and enhance a loved one’s quality of life for a limited period of time. Unfortunately, some of these prescriptions are only approved for use in cases of mild to moderate Alzheimer’s.”
Preventing Elder Abuse
“Even the early stages of dementia can be devastating, as demonstrated by my story about Rhonda, Sue and Jane. Elders who sound socially sufficient and seem to manage their daily routines relatively well seldom raise red flags. They are left in charge of their finances or in the care of another “trusted” family member. In this case, Sue said she wanted to be with her granddaughter instead of her daughter, and that seemed acceptable. Many seniors can put on a front and cover up changes in their mental functioning, so it can be difficult for family members to pick up on these changes (especially from afar). A physician can use a few specially formulated questions to read into a loved one’s level of awareness, ability to recall information and problems with basic skills such as language and mathematics.
“When I am trying to get a feel for a patient’s level of cognitive function, I ask thinks like, ‘What medical problems do you have?’ and ‘What medications are you on?’ If they cannot answer these questions, then they cannot take care of themselves, medically or financially. Another question I ask is a pretty simple math problem: ‘What is 25 percent of $22.50?’ If they cannot do that, they should probably receive help with their financial decisions. At this point, it is most important to bring in a trustworthy advisor or enforce their durable power of attorney (DPOA) if they were wise enough to prepare one in advance.
“One of the first mental impairments to occur with dementia is risk assessment. Therefore, the patient cannot properly assess when someone will help them or hurt them, or if a business deal is actually beneficial. It is not uncommon for abusers to take advantage of this and trick the person into signing over their home and assets. Since these opportunists are not particularly concerned about their victim’s wellbeing, it’s also not uncommon for them to wander off on foot and suffer from exposure or drive away and get lost. Some are found hundreds of miles from home.
“Exerting undue influence over an elder or keeping them away from outside family, friends and professionals who have their best interest at hand are telltale signs of abusive behavior. They often say things like, ‘Your kids will just put you in a nursing home and take your money, but I am here to keep you in your house.’ Or they will lie to outside professionals, for example accusing well-meaning family members of ‘inappropriate behavior’ when, in fact, they are the ones acting inappropriately.
“In scenarios like these, predatory activity has already taken place, and adult protective services (APS) must be contacted. However, APS is set up to handle physical abuse, safety issues, and financial elder abuse, not dementia diagnoses. Therefore, it is also wise to consult an elder law attorney and find a fiduciary to help with subsequent legal issues and financial management.
“Keep in mind that a loved one can still incur financial devastation without the ‘help’ of an abuser. Many dementia patients tend to spend frivolously, forget to pay their bills and make donations to charities and people that they cannot afford. An official diagnosis can help the entire family keep an eye on their general wellbeing and decision making to ensure nothing goes awry.”
An Answer Means More Than You Think
Dr. Landsverk’s compelling story is a warning for all of us. The earlier a person’s dementia is diagnosed, the more likely it is that trustworthy loved ones are involved to watch over their safety and wellbeing – both physical and financial. If you are noticing unusual behavioral or cognitive changes in your loved one, it is important to encourage them to see their primary care physician for a mini-mental state examination (MMSE) sooner rather than later. While it can be a difficult diagnosis to receive, this knowledge can empower you, your loved one and your family members to make informed decisions moving forward.
Dr. Landsverk has over twenty years of experience in providing medical care to the elderly. She is board-certified in internal medicine, geriatric medicine and palliative care. She founded ElderConsult Geriatric Medicine, a house calls practice, to address the challenging medical and behavioral issues that older patients and their families often face.

Elizabeth (Dr Liz) has over twenty years of experience in providing medical care to the elders. She is board-certified in Internal Medicine, Geriatric Medicine and Palliative Care Medicine. Dr Landsverk founded ElderConsult Geriatric Medicine, a house calls practice, to address the challenging medical and behavioral issues often facing older patients and their families.